Comparative Effectiveness Research Survey Course
- Addressing Disparities in Asian Populations through Translational Research
- Clinical Research
- Comparative Effectiveness Research Seminars
- Developing & Managing Your Research Career
- Drug and Device Development
- Good Clinical Practice (GCP)
- Grant Writing
- Health Communication
- Informatics
- NIH Biosketch, Policy, and Guidance Changes
- One Health
- Open House
- Pilot Studies Program
- Regulatory Affairs
- Research Coordinator Education
- Research Design and Data Analysis
- Research Process Improvement
- Research Recruitment and Participation
- Stakeholder & Community Engagement
- Survey, Qualitative & Mixed Methods
- T.5 Capacity in Medical Devices
- Team Science
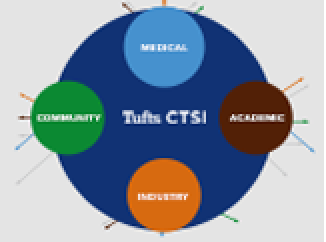
- Translational Science