Overview
As defined by the NIH National Center for Advancing Translational Sciences (NCATS), translation is “the process of turning observations in the laboratory, clinic, and community into interventions that improve the health of individuals and populations – from diagnostics and therapeutics to medical procedures and behavioral interventions.”
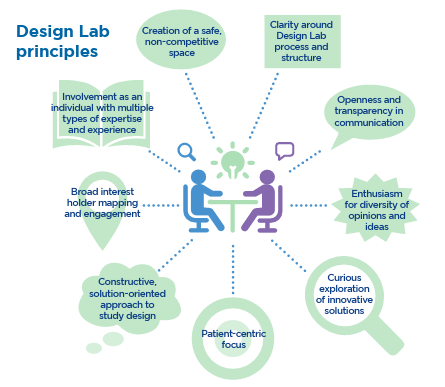
The process of translation is often lengthy and challenging. It involves both transforming an idea into a product or procedure through an intricate chain of development and testing activities and equally complex research needed to bridge the gap between those innovations and their implementation, broad adoption, and ultimate impact on health. This journey spans a broad spectrum of efforts, requiring the expertise and insights of many individuals, including patients, community members, and other stakeholders.
Translational science refers to systematic efforts to understand and address roadblocks commonly encountered in translational efforts. The aim is to generate scientific and operational innovations that transform the way that research is done, making it faster, and more efficient, and, thus, more likely to have an impact on health.
Defining the Translational Spectrum for Tufts CTSI
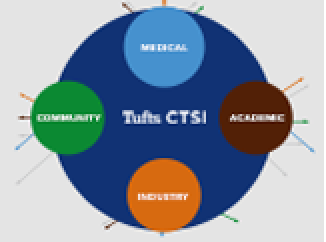
Tufts CTSI supports research across the full spectrum of translation, from initial proof-of-concept and pre-clinical testing to clinical trials and studies to support clinical implementation and public health programs. The process can be represented as involving five stages (T0-T4):
T0-T1: Bridging concepts and testable health applications. This stage is characterized by the transformation of concepts into testable applications, be they drugs, devices, diagnostics, or data algorithms.
- Example activities: Investigational New Drug (IND) and Investigational Device Exemption (IDE) studies; candidate gene studies
- Tufts CTSI supports: T.5 Capacity in Medical Devices Program; Research Studios
T1: Translation to humans. T1 involves early testing of candidate interventions or technologies in humans.
- Example activities: Phase 1 and 2 clinical trials; evaluation of novel diagnostic tools/methods
- Tufts CTSI supports: Tufts CTSI Clinical Study Centers; Regulatory Support Program; Informatics Program; Clinical Trial Design Labs
T2: Translation to patients. T2 involves the establishment of effectiveness in humans and the translation into health practice and clinical guidelines.
- Example activities: Phase 3 trials; controlled observational studies and other approaches to define the appropriateness of treatments and tests in clinical care.
- Tufts CTSI supports: Biostatistics, Epidemiology, and Research Design (BERD) Center; Recruitment and Retention Support Unit; Data Safety and Monitoring Board Program; Qualitative and Mixed Methods Service; Community Engagement Studios
T3: Translation to practice. T3 addresses the need to understand whether treatments, diagnostic tests, or other interventions are generalizable to the wider span of clinical practice.
- Example activities: Clinical studies in real-world settings; studies that include comprehensive clinical and patient-reported outcomes; dissemination research.
- Tufts CTSI supports: Dissemination and Implementation (D&I) Core; Comparative Effectiveness Research consultations
T4: Translation to the community and public health practice. T4 research translates effective health care delivery into improved community and population health, informs new policies, and includes interventions in, and monitoring of, populations.
- Example activities: policy evaluation; cost-benefit analysis; surveillance studies.
- Tufts CTSI supports: Community and Stakeholder Engagement consultations; Program Evaluation Service

Although presented as a linear series, the process should be understood as multidirectional and interactive, with work at each stage informing the others and often feeding back to basic science.
A graphic developed by NCATS captures this relationship while also emphasizing the centrality of patients at all stages of translation.