Designing an innovative research project isn’t just about building your resources; it’s also about understanding and maximizing the resources you already have. Rachael Bowers, LICSW, a pediatric social worker at the Dimock Center in Roxbury, MA, can certainly attest to this. Her participation in Tufts CTSI’s Building Your Capacity (BYC): Advancing Research Through Community Engagement Program (PDF) resulted in the creation of a novel research project which was recently mentioned in a New York Times article emphasizing the importance of recognizing and treating social determinants of health. As her research continues, she uncovers the potential for collaboration between clinical and community agencies to improve patient care efficiency.
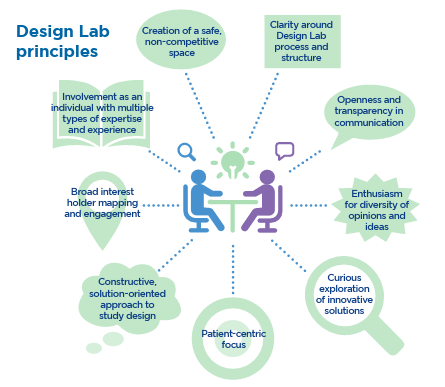
Before participating in Tufts CTSI’s BYC program, Ms. Bowers wanted to initiate more research at the Dimock Center but was unsure of how to answer the captivating research questions she had posed. “We loosely had the idea of what we wanted to look at, but I think that those first sessions on defining your question and refining it again and again until you have the very specific question that you potentially have the data to answer was a critical process,” she explains. The BYC program provides aspiring investigators or fellows with funding and valuable training for the conduction of community engaged research, which involves community members in any stage of the research process. The program provides two levels of support to aspiring investigators. Training sessions help clarify the process of establishing academic community partnerships, understanding ethics, developing and refining a research question and selecting an appropriate study design. Each fellow is subsequently paired with a research consultant, who provides guidance throughout all stages of project development. Fellows are specifically instructed to develop projects that are relevant to their professional work. Carolyn Leung, EdD, MA, Program Manager, Aligning Researchers and Communities for Health (ARCH) at Tufts CTSI and Assistant Professor at Tufts Medical Center, explains, “We provide a framework, but we really want it to be led by the community partner so it meets one of their organizational needs.” Bearing this in mind, Ms. Bowers strived to measure the outcomes of recent social work at the Dimock Center while also considering her professional interests in the process of creating her project.
After partnering with Health Leads, an organization which helps recruit student volunteers at hospitals and community agencies to connect patients with basic resources, in October, 2010, Ms. Bowers noticed a vast improvement in the efficiency of Dimock Center social workers and wanted to investigate the enormity of the organization’s impact. Her first aim was to define her role as a social worker at the community health level, working in a medical health setting but not as a primary care therapist. She admits, “I had a concern that their [the students’] work could be confused for clinical social work in a medical setting.” To capture the accomplishments of Dimock Center social workers before and after the partnership, Ms. Bowers and her research team compiled four years of patient referral data logged by Dimock Center social workers and compared this with data collected by Health Leads on familial needs and amount of resource connections successfully made.
What they found was the Dimock Center’s referral output rate had more than doubled for the basic needs of the families they serve after partnering with Health Leads, revealing an enormous effect on the agency’s competency. As Health Leads volunteers are able to take on more basic cases, Dimock Center social workers can devote more time to patient care. For Ms. Bowers and her team, this is only the beginning. With the partnership extending through next year, she anticipates, “The second year will be more successful because of the learning curve, both for us and for the students.” She predicts that a secondary project outcome may be revealed from the data, which could show that general clinical referrals for mental health, including school-related and developmental needs, have also increased as a result of the partnership. She explains, “As Health Leads came in, my case load expanded and we have been able to offer services faster and in a familiar setting to our patients.” Eventually, she hopes to measure whether the expanded therapy and pediatric care services at Dimock have resulted in any community health outcomes, such as improved mental health because of more efficient and less repetitive medical appointments.
Elaborating on the BYC program’s integral contribution to her project’s continuing success, Ms. Bowers says, “In terms of timelines, it [the program] couldn’t have been more in sync with how the concept of our research was being developed . . . It didn’t just help us to build our capacity, but to understand our capacity, because some of it we were doing without realizing what we were doing.” Her project provides just one example of the capacity community agencies have to transform medical care, shifting focus from disease itself to the social factors that contribute to disease. “One thing I really appreciate about Rachael’s project is that it combines the clinical aspect of care with the social determinants of health, and helps us to understand the necessary linkage of these conversations,” Dr. Leung comments. “We provide the opportunity for people to stop and think about how they can move their work to the next level.”